WITH nearly 30 years as an NHS consultant and as a British Asian woman, I am acutely aware of the unique challenges ethnic minority patients face in healthcare, especially on their journey towards parenthood.
This week, National Fertility Awareness Week shines a critical light on the psychological impact of infertility in minority ethnic communities. It is time to confront the barriers and stigmas contributing to inequalities in IVF access and outcomes for BAME patients, and the ways these amplify the mental challenges in what is often already a highly emotional and personal journey.
Recent data from the Human Fertilisation & Embryology Authority (HFEA) revealed that black and Asian patients consistently experience the lowest birth rates in IVF treatment. Indeed, the average IVF birth rate using fresh embryo transfers among patients aged 18-37 was 24 per cent for Asian patients, compared to 32 per cent for white patients.
The disparities impacting BAME patients’ access to fertility treatments and their outcomes are multifaceted. Factors including pre-existing health conditions that can impact fertility, along with economic, social, cultural and structural factors – including persisting stigmas in some communities – all contribute to the obstacles that hinder open dialogue and equitable access to care.
It appears that at every step along the fertility treatment journey, women from ethnic minority communities face disparate challenges that can increase infertility related emotional distress. For example, Asian women tend to be more prone to polycystic ovarian syndrome (PCOS), a condition that can lead to extended delays in treatment due to NHS waiting lists, subsequently prolonging referrals for IVF. Additionally, PCOS is often associated with a higher BMI, which can affect IVF eligibility and lead to further delays.
With the biological clock impacting fertility for both men and women, earlier diagnosis of underlying health conditions and accessible treatment can make the difference when it comes to a successful IVF outcome.
Compounding these issues, a 2021 HFEA report highlighted that 52 per cent of Asian couples seeking IVF had to rely on white donor eggs, as only four per cent of egg donors are of Asian descent. Many patients feel it is essential for the donor’s ethnicity to match their own, resulting in additional treatment delays and potentially poorer outcomes.
Economic factors also play a significant role. The Women’s Health Strategy highlighted disparities in NHS funding and provision of fertility treatment across England, with BAME communities relying more on NHS-funded treatment.
Geeta NargundUnfortunately, the NHS postcode lottery disproportionately impacts these groups, leading to delayed diagnoses for infertility-related conditions and hindered access to treatment. It is essential we tackle the NHS postcode lottery to improve accessibility of IVF, ensuring funding options are available for every individual who needs additional financial support so they can access the treatment they need.
Yet often one of the greatest factors increasing the mental toll amongst patients from ethnic minority communities facing fertility challenges is the enduring stigma that surrounds infertility and fertility treatments. I often hear from Asian patients and As-ian patient support groups that there is unfortunately still a stigma associated with infertility and fertility treatments. Sadly, many patients can feel isolated and unable to share their experience of treatment with their friends and family. It is essential that we raise awareness and tackle the taboos surrounding infertility.
There is still the common view that infertility is solely a ‘women’s issue’, which is entirely false – around half of all cases of infertility are due to a male factor. By educating Asian communities and raising awareness, we can help tackle taboos and make it easier for those suffering from fertility problems to have open conversations about their experiences, creating a supportive environment for them while they go through fertility treatments.
Ultimately, tackling these disparities requires a collaborative effort. We must raise awareness and understanding of fertility issues among ethnic minority communities, through community networks and patient support groups. We must also reduce NHS waiting lists for the initial diagnosis and treatment of pre-existing reproductive health conditions, alongside ending the NHS postcode lottery, which is resulting in disparities of access to funded IVF treatment across the country.
By opening up the conversation around infertility and addressing the stigmas that persist, we can level the playing field and improve both access and outcomes for BAME patients on their journeys towards parenthood.
Professor Geeta Nargund is the awardwinning medical director of abc ivf. She is also the medical director of CREATE Fertility, sister clinic, and a senior consultant gynaecologist and lead consultant for reproductive medicine services at St George’s Hospital, London.





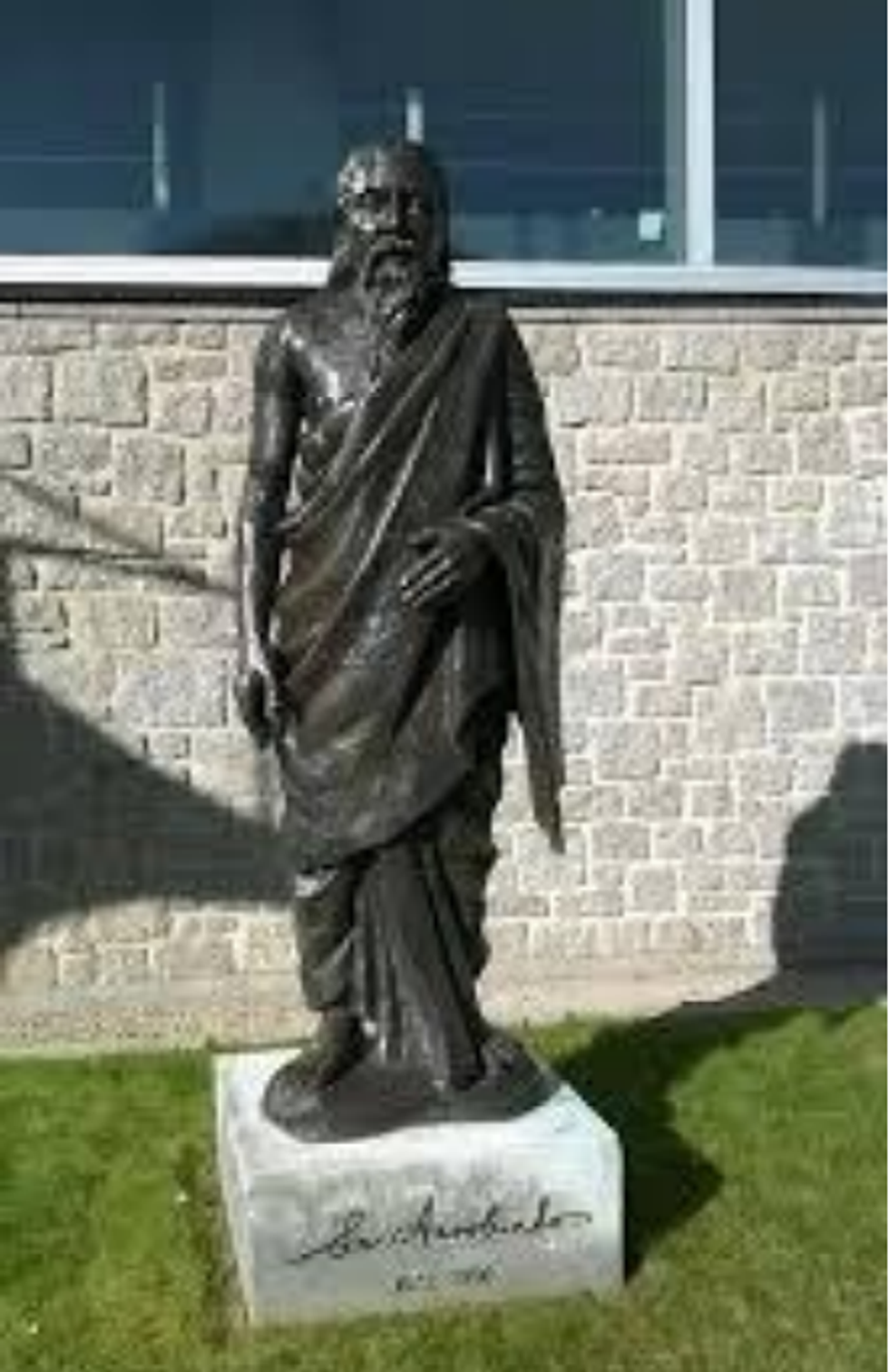 Heehs describes two principal approaches to biographyAMG
Heehs describes two principal approaches to biographyAMG












 David Beckham wearing a David Austin Roses "King's Rose" speaks with King Charles III during a visit to the RHS Chelsea Flower Show at Royal Hospital Chelsea on May 20, 2025Getty Images
David Beckham wearing a David Austin Roses "King's Rose" speaks with King Charles III during a visit to the RHS Chelsea Flower Show at Royal Hospital Chelsea on May 20, 2025Getty Images
‘Ethnic disparities in IVF success rate highlight access challenges’
Minorities delay fertility care amid social stigma and economic barriers